- Dentists play a critical role in screening patients for risk factors of sleep-disordered breathing.
- CBCT can generate high-quality airway imaging even with low-dose exposure.
- The diagnosis of sleep disorders is done by medical doctors and aided by dental CBCT imaging.
- Official CBCT Reports written by Oral & Maxillofacial Radiologists serve to educate patients about their sleep apnea risk and facilitate efficient referrals to medical doctors.
Airway assessment has been simplified by the advent of cone beam computed tomography (CBCT) technology. CBCT is a readily accessible modality clinicians can adopt to analyze airway morphology, volume, and pathology. This information is integral to the diagnosis and treatment of various airway disorders, including obstructive sleep apnea (OSA) and upper airway resistance syndrome (UARS). Effective and appropriate use of CBCT in airway analysis will be discussed.
Understanding the scope of practice as defined by the American Academy of Dental Sleep Medicine (AADSM) is an important first step. Dentists can obtain the knowledge and resources to screen patients for OSA, however, the DIAGNOSIS is made by a physician through questionnaires, physical examination, and the results of a sleep study. Dentists may participate in the management of the condition through oral appliance therapy (OAT) as an alternative to continuous positive airway pressure (CPAP) units, both of which must first be prescribed by the physician. This article will focus on the screening process and the role of CBCT imaging.
In most practices, it is both unnecessary and inappropriate to screen all patients with CBCT. Patients should first be screened through medical history and sleep questionnaires. Those with risk factors and symptoms of OSA, even if not yet diagnosed by a physician, may be suitable for a CBCT. The scan exposure parameters should be specific to the patient and study to be acquired. Large volume scans are necessary to incorporate all the regional anatomy, so utilizing low-dose exposure settings is good practice and aligns with the principles of ALADA / ALARA.
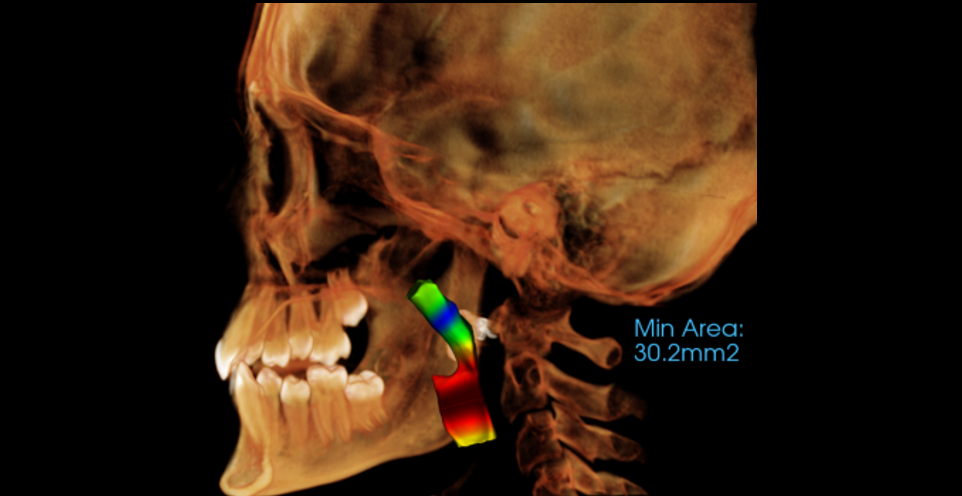
Once the CBCT scan is complete, the next step is to perform airway analysis. Image viewing software commonly contains tools for measuring airway volume and cross-sectional area. These measurements are then interpreted via comparison with normal ranges, which can vary by age. Even still, subjectivity plays a role. In practice, CBCT scans for other treatment needs such as wisdom tooth extraction may demonstrate a narrow airway relative to “normal”, though the patient has neither risk factors nor symptoms.
Airway volume is a parameter that defines the amount of air the passageways may support at a given time. Low airway volume is a risk factor for sleep-disordered breathing and may be exacerbated by things like enlarged tonsils or the presence of other pathology. Cross-sectional area assessment can localize abnormalities, typically identified in the axial or sagittal planes. Asymmetry in the soft tissue may highlight areas worthy of further investigation, especially in the presence of other risk factors.
To avoid false positives and false negatives when measuring airway dimensions, proper patient positioning and instructions must be adhered to. Positioning – the patient’s head and neck must be aligned and centered via adjustment of the gantry height to allow for an upright spine. This should be done prior to positioning the patient and before dialing in once they are in place. The up/down positioning of the head is correct when the Frankfurt horizontal plane is parallel to the floor, and the left/right positioning is correct when the mid-sagittal plane is perpendicular to the floor. The neck position is optimized by extending it as much as can comfortably be achieved while dropping the shoulders inferiorly, the combination of which will allow the gantry to freely rotate around the patient. If not done correctly, there will be exaggerated cervical spine curvature and potential patient contact by the gantry resulting in movement artifact. Instructions – just prior to acquiring the scan, the patient should be told to “close your eyes, swallow one last time, and keep your tongue at the roof of your mouth.” These directions combined with correct positioning will ensure the airway and surrounding musculature are in a neutral position, there is no patient movement, and the measured airway dimensions will be an accurate baseline on which to make diagnostic determinations and/or compare to post-treatment as applicable.
Skeletal abnormalities and asymmetries that may contribute to airway disorders can also be identified. Enlarged nasal turbinates, hypoplastic sinuses, and deviated nasal septa can restrict airflow. Tumors, cysts, and inflammatory pathology may also be depicted. These conditions can lead to dangerous airway obstruction. CBCT allows clinicians to visualize these structures in any plane and in 3-D, and the data can be easily shared with ENT specialists and Oral Surgeons. With early detection, appropriate referral and life-saving intervention can be accomplished.
In the event OAT is prescribed, fabricated, and fitted, a follow-up low-dose CBCT scan can be acquired with the appliance in place. Whether designed to reposition the mandible, displace the soft palate, or for any other suitable purpose, this scan should demonstrate improvement in cross-sectional area and airway volume. Ideally, the patient will report subjective improvement in the signs and symptoms of sleep-disordered breathing. A follow-up sleep study can also be done for objective analysis.
If soft tissue pathology is suspected, other imaging protocols may be needed since CBCT has poor soft-tissue contrast – the use of MRI or multi-detector CT will provide more detail regarding the nature and extent of the lesion in question. However, CBCT is still advantageous for surgical planning (due to ability to highlight osseous anatomic landmarks) and screening those at risk for sleep apnea (due to significantly lower radiation dose).
By visualizing the airway in 3-D and comparing the findings with established normal ranges, Oral & Maxillofacial Radiologists can help dentists effectively screen patients at increased risk for sleep-disordered breathing. Considering the comorbidity with heart disease and other health conditions, early detection will predispose these patients to improved length and quality of life.